.. by Mike Moffitt
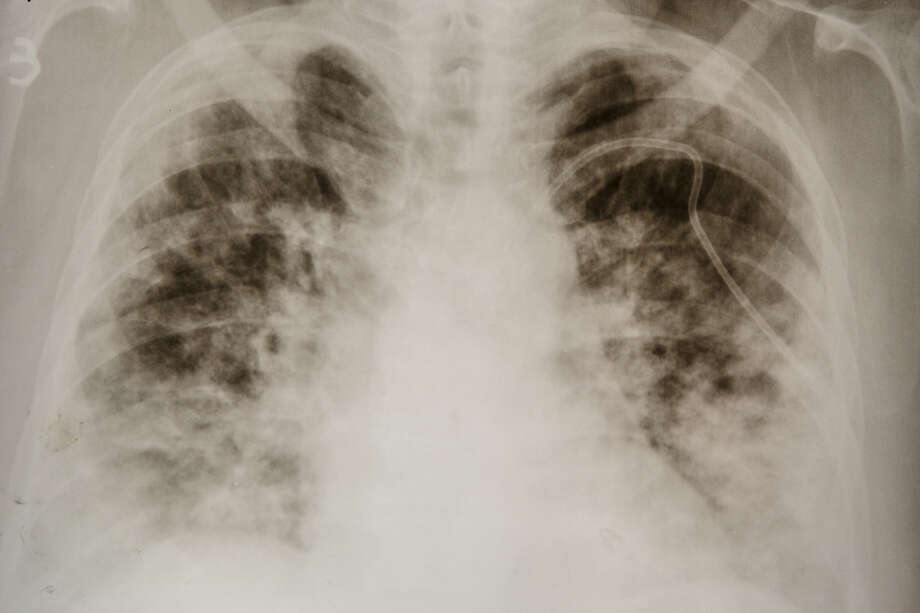
A chest X-ray of a COVID-19 patient shows “consolidation,” a radiological term refering to dense opacities obscuring lung vessels and bronchial walls. (File photo from the Zakarpattia Centre of Lung Diseases, Uzhhorod, western Ukraine,
Most people who catch the new coronavirus don’t experience severe symptoms, and some have no symptoms at all. COVID-19 saves its worst for relatively few.
ICU nurse Sherie Antoinette has seen the serious cases first hand.
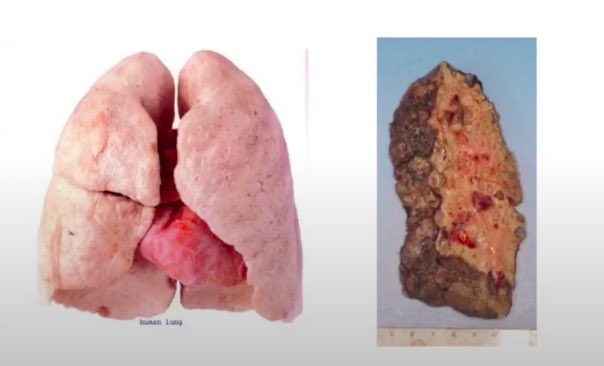
The lucky ones — if you can call them that — recover, but not in the sense that their lives are back to normal. For some, the damage is permanent. Their organs will never fully heal.
“When they say ’recovered,’ they don’t tell you that that means you may need a lung transplant,” Antoinette wrote in a Twitter post. “Or that you may come back after discharge with a massive heart attack or stroke, because COVID makes your blood thick as hell. Or that you may have to be on oxygen for the rest of your life.”
COVID 19 is the worst disease process I’ve ever worked with in my 8 years as an ICU nurse.When they say “recovered” they don’t tell you that that means you may need a lung transplant. Or that you may come back after d/c with a massive heart attack or stroke bc COVID makes
We have selected some of their tweets and are running them with minor editing for clarity. SFGATE makes no claims to their authenticity.
I’m currently in the hospital after having a heart attack caused by clotting that resulted from COVID 19. I have a stent in my heart and need to wear a heart monitoring vest at all times. Now I face months of recovery including physical and occupational therapy. I’m only 29.
I went into acute kidney failure and needed dialysis. I now have asthma, chronic cough and an irregular heartbeat. I have conditions I never had before, plus I’m wiped all the time. I hope this gets better, but you [Sherie] are on the money. And, mine was considered a low-moderate case.
— Stephanie McCarroll
These are my observations (of hospitalized patients):
1) Everybody is so swollen their skin has blisters and is so tight it looks like it’s about to burst, from head to heel. And skin so dry peeling and flaky that to slather Vaseline on every shift is almost necessary — all over.
2) Everybody’s skin is weeping clear fluid and has sores and the skin just slides off with slightest turn or rub, all over the body.
3) Everybody’s blood is thick as slush. Can’t figure out what’s making it clot like that, but it’s dark and thick.
4) Everybody’s kidneys are failing. Urine dark or red, which could contribute to the swelling, but we don’t know yet.
5) Everybody has an abnormal heart rhythm. Not sure of the cause. But even without underlying heart problems, it’s not beating normally.
6) Seems counterproductive, but the ones that are not breathing on the ventilator have to lay flat on their stomachs to breathe better. And even some on the ventilator are on their stomachs. And the slightest turn for some is what leads to their almost immediate death. Bathing, cleaning and turning to prevent skin breakdown causes most to code blue, so a decision has to be made on which is most important.
7) Everyone has a Foley catheter and a rectal tube — incontinent of bowel and bladder.
8) Everybody on tube feeding. Everybody.
Never before in my entire career have I seen a disease process attack in this way.
— 20-year veteran nurse in NYC via Dr. Dee Knight

I spent 10 days on a ventilator last March with ARDS [Acute Respiratory Distress Syndrome] and I’m still on oxygen. Going home is just the beginning of the next steps in recovering. Every aspect of my life has changed for the worse. Please support and help anyone you know who survived. And wear a mask!
— Nurse @liveV4Vendetta
I’m just getting over a “mild” case after over two months. There’s scarring in my lower right lung and my stomach and digestion are a mess like never before. But I’m coughing way less and can take walks again.
And, btw, this is the third time in two months that I’ve “gotten better.” I’m just hoping it’s the last and it doesn’t all come back AGAIN.
— Eli
I’m a nurse on a COVID floor, I caught it. I am a relatively healthy 24-year-old and could barely walk up a half flight of stairs. My blood pressure skyrocketed, chest pain was debilitating. I’m 8 weeks out and still feeling the chest pain and shortness of breath. This is no joke.
— Alicia
I had COVID for over 60 days. I’m 33 years old, was super healthy, pescatarian, 125 pounds, and ran and did yoga every day. I couldn’t walk for two weeks besides a couple steps. It was the worst illness of my life.
I didn’t realize I had COVID symptoms for weeks. Here were the early signs:
– Waking up sweaty (I normally don’t sweat at night).
– Slight sporadic chills but no fever (or I thought I had no fever bc I only took my temp during the day).
– I could smell fine but would have weird smells like metallic or gas. Also, tasted metallic in the past 2-3 weeks. Apparently, a metallic taste or smell is related to lung problems.
– Loose stool but not terrible.
— Covid teacher (To read more about her symptoms and treatment, see her blog.)
I “recovered” March 29. I was born 65 years ago with chronic bronchitis that usually popped up maybe twice a year. Now, after COVID-19, I have acute bronchitis attacks 3-4 times a month and get winded walking to the mailbox.
— Hollis Charles
COVID 19 is the worst disease process I’ve ever worked with in my 8 years as an ICU nurse.
When they say “recovered” they don’t tell you that that means you may need a lung transplant. Or that you may come back after d/c with a massive heart attack or stroke bc COVID makes
jeanne fisher@jeannefisher17
— @PinkkYaYa
My mom worked on a COVID ward and contracted it, spent a month in ICU. She’s lucky enough to be home now, but she struggles to get up stairs and it’s going to be a long road to recovery. Thank you for everything that you do.
— Leanne
My coworker — an otherwise totally healthy 30-year-old — is still having issues breathing, two full months later. We’ve got patients coming back to the ER after they’re “recovered” because they can’t breathe or they get a blood clot. It’s so insane.
— Andi
I had it back in March and did 6 days on a ventilator. To date, I’m still short of breath with little exertion. I have pains all over that I have never had before. I’ve noticed I don’t urinate as much as I use to. And my legs & feet keep swelling so large no shoes fit. Even flops.
— Melly B.
I’m a healthy, active 23 year-old and I still have significant lung damage two months after I’ve “recovered.”
— Laney Whitney
Yeah, my mom “recovered” mid-May, except she had *nothing* left. Couldn’t even eat or drink, they wanted to surgically insert feeding tube into her stomach. I had to invoke her DNR instructions, that SUCKED. She passed May 25. Thanks for all you do, be safe, good luck.
— @DevinCojones
Worst sickness ever. Left me and my husband sick and weak for almost two months. Almost killed my perfectly healthy 41-year-old nephew. Took down a 36-year-old friend with two bouts of pneumonia. Wear a freaking mask, people. How hard is that?
—Padma’s mom
My husband and I caught COVID two and a half months ago. While my symptoms were mild, he nearly had to be admitted because he couldn’t breathe, and now, a month after he’s recovered, we’ve discovered he has PERMANENT LUNG DAMAGE.
This is not “just the flu.” It isn’t.
— Sue Mii
I had a “mild” case in February. I wasn’t hospitalized. Still extremely ill with a myriad of symptoms, including inflammation and lots of pain for 3 weeks. I have no doubt this virus causes permanent damage. Talk with someone who’s had it before you decide to go without a mask.
— Leicia Faye
.. SOURCE